Introduction
Among the numerous complications associated with diabetes, one of the most concerning is diabetic retinopathy, a condition that can lead to vision impairment and even blindness if left untreated. Despite its serious nature, diabetic retinopathy is preventable and manageable with proper care and attention.
What Is Diabetic Retinopathy?
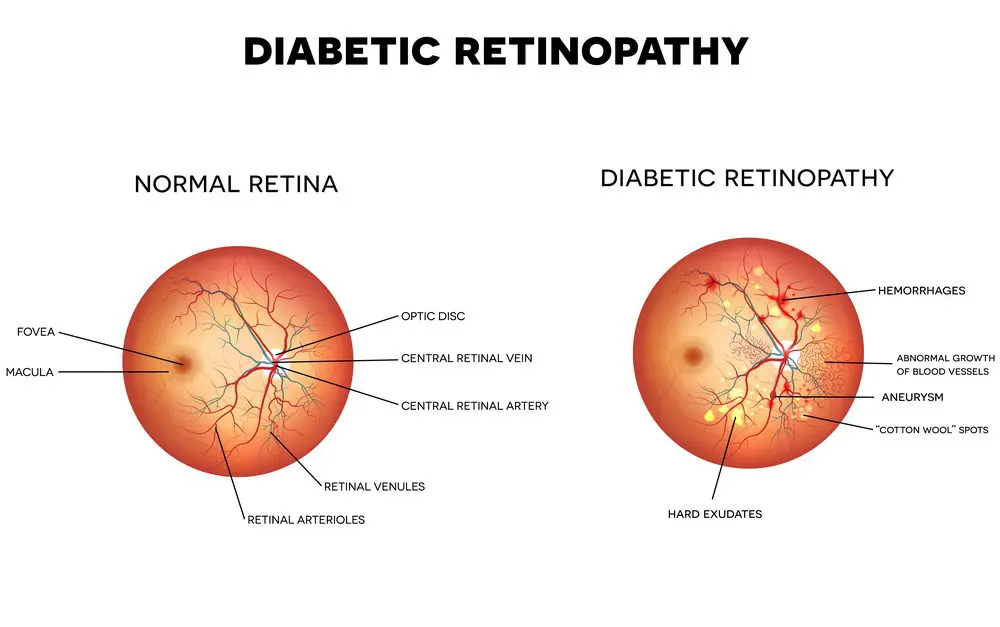
Diabetic retinopathy is a diabetes-related complication that affects the eyes. It occurs when persistently high blood sugar levels damage the blood vessels in the retina, the light-sensitive tissue at the back of the eye. Over time, this damage can lead to fluid leakage, swelling, and abnormal blood vessel growth, impairing vision. Diabetic retinopathy is one of the leading causes of blindness among working-age adults, but early detection and treatment can significantly reduce the risk of severe vision loss.
How and Why Does Retinopathy Develop in People with Diabetes?
- High Blood Sugar and Blood Vessel Damage: Chronic high blood sugar levels can damage the retina’s small blood vessels (capillaries). This damage weakens the walls of the blood vessels, making them more prone to leakage and rupture. As a result, the retina’s ability to function properly is compromised.
- Stages of Diabetic Retinopathy:
- Mild Non-Proliferative Retinopathy: This early stage is characterized by small bulges in the blood vessels (microaneurysms), which may leak fluid and cause retinal swelling.
- Moderate Non-Proliferative Retinopathy: At this stage, the blood vessels supplying the retina are further damaged, restricting blood flow.
- Severe Non-Proliferative Retinopathy: Blocked blood vessels deprive areas of the retina of oxygen and nutrients, releasing signals that promote abnormal blood vessel growth.
- Proliferative Diabetic Retinopathy: This advanced stage involves the growth of new, fragile blood vessels on the retina and into the vitreous (the gel-like substance in the eye). These vessels are prone to bleeding and can lead to scarring, retinal detachment, and vision loss.
- Macular Edema: Diabetic macular edema (DME) is a common complication of diabetes causing fluid to leak into the macula, the central part of the retina responsible for sharp vision. This leads to swelling and blurred or distorted vision
- Risk Factors:
- Poor blood sugar control
- High blood pressure
- High cholesterol
- Long duration of diabetes
- Smoking
- Pregnancy (in women with diabetes)
How Is Diabetic Retinopathy Diagnosed?
Early detection is crucial in managing diabetic retinopathy and preventing vision loss. Regular eye exams are the cornerstone of diagnosis. Here are the common diagnostic methods:
- Comprehensive Eye Examination: An eye specialist (ophthalmologist) will perform a thorough eye exam, which includes dilation of the pupils to examine the retina and blood vessels.
- Fundus Photography: High-resolution images of the retina are captured to identify signs of diabetic retinopathy, such as microaneurysms, hemorrhages, and abnormal blood vessels.
- Optical Coherence Tomography (OCT): This imaging test provides cross-sectional images of the retina, allowing the doctor to detect swelling and fluid accumulation.
- Fluorescein Angiography: A fluorescent dye is injected into a vein, and photographs of the retina are taken as the dye travels through the blood vessels. This test highlights areas of leakage or abnormal vessel growth.
- Vision Tests: Visual acuity tests are conducted to assess the impact of diabetic retinopathy on vision.
How to Prevent and Manage Diabetic Retinopathy
While diabetic retinopathy is a serious condition, there are effective strategies to prevent and manage it. Taking a proactive approach can significantly reduce the risk of complications.
Prevention
- Maintain Optimal Blood Sugar Levels: Keeping blood sugar levels within the target range (HbA1c < 6.5 or 7%) reduces the risk of damage to retinal blood vessels. Work closely with your healthcare team to develop a personalized diabetes management plan.
- Control Blood Pressure and Cholesterol: High blood pressure and cholesterol can exacerbate retinal damage. Regular monitoring and appropriate medication can help keep these factors under control.
- Adopt a Healthy Lifestyle:
- Diet: Follow a balanced diet rich in vegetables, fruits, whole grains, and lean proteins. Limit sugar, processed foods, and saturated fats.
- Exercise: Engage in regular physical activity to improve overall health and help manage blood sugar levels.
- Quit Smoking: Smoking accelerates blood vessel damage and increases the risk of diabetic complications.
- Regular Eye Exams: Annual comprehensive eye exams are essential for early detection and monitoring of diabetic retinopathy. More frequent check-ups may be necessary for those with advanced stages of the condition.
Management
- Medications:
- Anti-VEGF Therapy: These medications inhibit vascular endothelial growth factor (VEGF), reducing abnormal blood vessel growth and swelling.
- Steroid Injections: Corticosteroids may be used to reduce inflammation and retinal swelling.
- Laser Treatment:
- Focal Laser Treatment: Targets specific areas of leakage in the retina.
- Pan-retinal Photocoagulation: Reduces abnormal blood vessel growth by treating a broader area of the retina.
- Surgery:
- Vitrectomy: This procedure involves removing the gel-like vitreous from the eye to address severe bleeding or retinal detachment.
- Blood Sugar, BP & Cholesterol Management: Improved sugar, BP & Cholesterol control, slow the progression of diabetic retinopathy and enhance the effectiveness of treatments.
- Regular Monitoring: Follow-up appointments with an eye specialist are critical to track disease progression and assess treatment outcomes.
Conclusion
Diabetic retinopathy is a serious but preventable & manageable complication of diabetes. By understanding its causes, recognizing its symptoms, and adhering to a proactive prevention and management plan, individuals with diabetes can significantly reduce their risk of vision loss. Regular eye exams, optimal blood sugar, BP, Cholesterol control, and a healthy lifestyle are the cornerstones of preventing diabetic retinopathy. If you have diabetes, prioritize your eye health and consult an eye specialist for regular screenings. With early detection and appropriate care, you can protect your vision and maintain your quality of life.